WHO ARE WE?
Androlabs is the first global pharmaceutical company dedicated to men’s health. Headquartered in London, our mission is to close the male life expectancy gap. We are responsible for two prescription medicines for men’s health, which have been used more than 6 million times by patients across Europe in recent years.
We have spent the last 3+ years engaging daily with top andrologists (clinical specialists for men’s health), endocrinologists, urologists and GPs across Europe. To illustrate further our good fortune – our Scientific Advisory Committee’s most recent report was just published in the world-famous Andrology journal. These relationships have given us incredible insights into overlooked men’s health issues and have helped us on our journey to provide more products and services that help improve the overall wellbeing of men.
EXECUTIVE SUMMARY
We have highlighted three opportunities that we believe the UK Men’s Health Strategy should take into account, to help reduce the male life expectancy gap and build an NHS fit for the future:
- Creating a men’s health qualification for healthcare professionals to improve patient outcomes
- Broadening screening and treatment incentives for men’s health conditions to combat key drivers of premature male mortality
- Establishing a dedicated men’s health research team to both drive and report improvements in men’s health across the UK
Firstly, we believe the creation of a men’s health qualification for healthcare professionals would help combat the stigma, myths and uncertainties regarding men’s health topics. It would also help to address the fact that male health topics currently have a very limited role in healthcare professional training. This qualification needs to be designed carefully to appeal to GPs, due to the key role they need to play in connecting the dots between the different silos of specialties that men need to engage with on their healthcare journeys.
Secondly, we are strong proponents of two expressions: “You can’t manage what you don’t measure” and “Show me the incentives and I’ll show you the outcome”. We see value in broadening the current scope of screening and incentives addressing men’s health conditions. We suggest that screening, diagnosis and treatment of some key drivers of premature male mortality could be supported to great effect – for example, prostate cancer, low testosterone and erectile dysfunction.
“You can’t manage what you don’t measure.” We propose that a dedicated men’s health research team be established to set new standards for data quality and measure impact of different initiatives. This way, ambitious, numbers-based targets can be included in the men’s health strategy and tracked, distinguishing it from the men’s health strategies of Australia, Ireland and others.
We believe seizing these opportunities will create a virtuous cycle of ever more effective initiatives, leading more men to get screened and treated by confident healthcare professionals, thereby addressing key drivers in premature male mortality.
We at Androlabs want to leverage our network of healthcare professionals across Europe to support the delivery of a successful Men’s Health Strategy. We would be excited to conduct surveys and interviews to identify other best-in-class practices. We fully support the government’s ambitions around a ten-year approach to men’s health, and this submission has been developed in partnership with that goal in mind.
1. What are the challenges we see driving the male life expectancy gap?
The main conditions that cause premature male mortality are well-known, as are their main drivers. Highlighting that heart disease, and its core drivers like obesity, lack of exercise, and high blood pressure, are important to address is not impactful.
Stating that increasing men’s access to healthcare (either by providing it in more convenient or more appealing spaces, or at more convenient times) will improve outcomes is also not impactful. We will avoid postulating about optimal GP resourcing and compensation.
Below, we highlight six key challenges that we have clear visibility of and are convinced the UK Men’s Health Strategy should take into account. These six challenges prevent a typical man’s health journey from being as successful as it should be, and in turn drive the male life expectancy gap.
1A. Men are not being referred properly in a siloed system of healthcare professionals, leading to under-treatment
1B. GP awareness of and confidence in treating men’s health conditions is low, leading to under-treatment
1C. The “Over 40s Healthcheck”, one of the first healthcare touchpoints for many men post-adolescence, doesn’t include key tests for PSA and testosterone
1D. GPs are not incentivised to follow up on key men’s health conditions, even those that are key drivers of premature male mortality
1E. There is a growing amount of misinformation online, while online channels play a greater and greater role at the beginning of the male health journey
1F. There is a lack of good quality data available to assess the impact of men’s health initiatives, which limits the ability to express their return on investment if scaled
More details are provided below.
1A. Men are not being referred properly in a siloed and fragmented system of healthcare professionals, leading to under-treatment
Below is an overview of an illustrative health journey for a man with very typical health conditions.
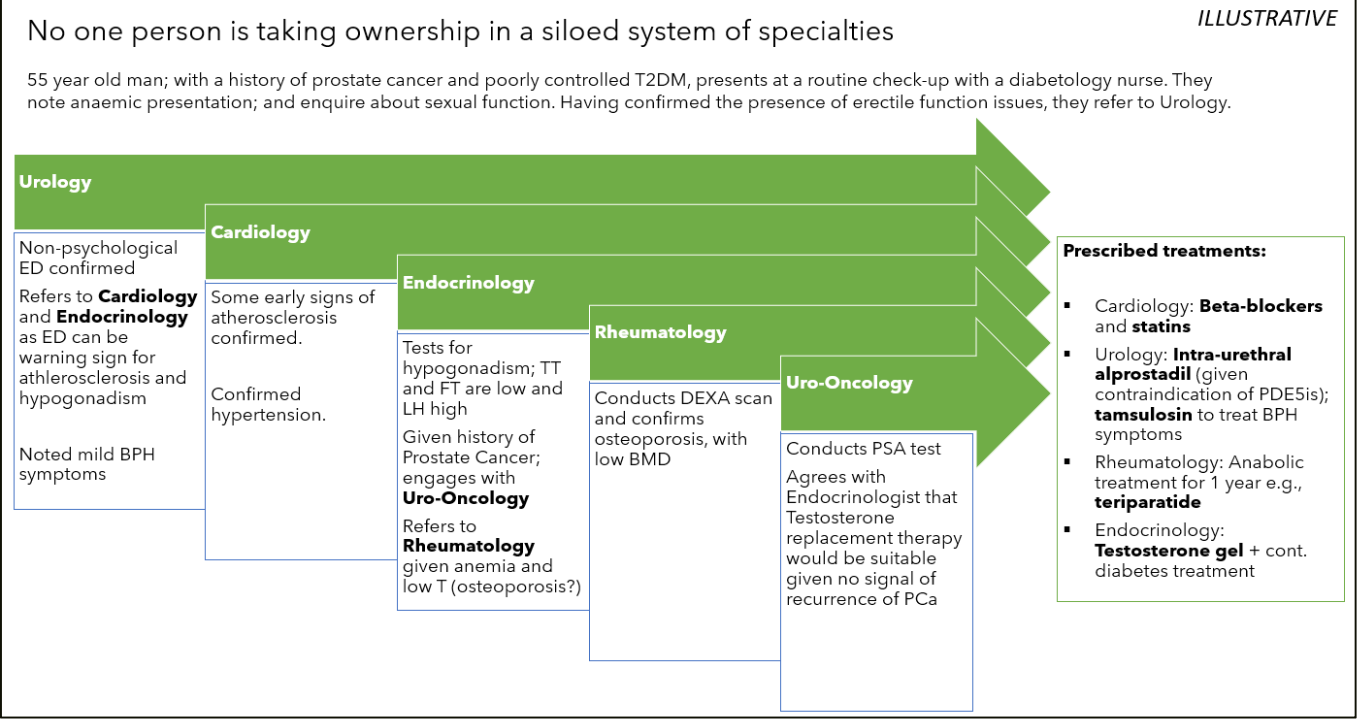
From our conversations with thousands of specialists across the UK and Europe, we can confidently say that these and other life-changing onward referrals are not being made consistently. For example:
- Even when men are treated for bone fractures, few are tested for osteoporosis – perhaps due to its reputation as a “women’s condition”. This may explain why men account for 40–50% of the deaths due to fractures, despite a much lower prevalence.
- Erectile dysfunction is an early warning sign for cardiovascular disease; however, sexual topics are still avoided by specialist and patient alike, while onward referrals to cardiology are rarer still.
1B. GP confidence in treating men’s health conditions is limited due to a lack of structured andrology training
Well-known specialists have confided in us that the time spent training on andrology topics in the GP curriculum can be as little as one afternoon – which pales into insignificance compared with other topics, e.g., obstetrics.
The education of GPs and junior doctors on andrology topics is not well monitored nor well structured. The type and volume of training is heavily dictated by the existence, availability and biases of local specialists.
We propose that the lack of structured andrology training, as seen in other European countries, limits interest in andrology specialisations, creating a vicious cycle of access and education. Is it any surprise that there is not a Royal College of Andrology?
As referenced above, there is still an element of stigma around the treatment of men’s health conditions, especially those related to sexual function and hormones. When combined with access and education issues, the potential for men’s health conditions to be under- or misdiagnosed increases.
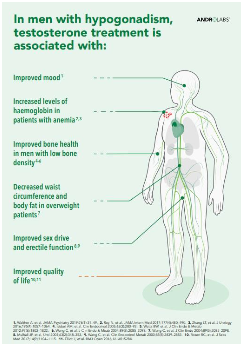
We believe this is a key driver in the systematic underdiagnosis of low testosterone (also known as hypogonadism, or testosterone deficiency). Some estimates put the treatment rates of low testosterone at just 10–12%, which is remarkable for a condition that is proven to drive increased mortality, impacts every cell in the body and exacerbates or causes many other debilitating conditions.
1C. The “Over 40s Healthcheck” doesn’t include key tests for PSA and testosterone
The Over 40s Healthcheck is a critical moment in a man’s health journey. It is, for many men, the first healthcare touchpoint they will have had since adolescence. Surprisingly, focus is put on thyroid testing – which is a more expensive test than that for testosterone and focuses on a condition which is rarer than prostate cancer.
1D. GPs are not incentivised to follow up on key men’s health conditions
We are proponents of the expression “Show me the incentives and I’ll show you the outcome.” Testing and treatment of erectile dysfunction is not incentivised as it was before. This change in focus has led to a dearth of erectile dysfunction clinics across the country.
This is a worrying statistic, given that erectile dysfunction has been proven as an early warning sign for cardiovascular disease – one of the main contributors to premature male mortality. Cardiovascular disease is so often a “silent killer”.
Our analysis of the number of erectile dysfunction prescriptions in the UK shows a flatline over the last year – a surprising figure given the increasing age, weight and levels of ill health of the general population. This implies the condition is underdiagnosed and undertreated.
1E. Misinformation online is increasing while online channels play a bigger role
Men are increasingly leveraging the internet for health advice. The misinformation and mixed messages available online lead to real-life sub-optimal health outcomes.
1F. Lack of good quality data limits assessment of initiative impact
Another expression we are fond of here at Androlabs: “You can’t manage what you don’t measure.” The volume and quality of data regarding men’s health and supporting initiatives is very poor. This makes it challenging to set, let alone track, clear metrics of success. This lack of clarity is likely the cause of the general lack of figures in existing men’s health strategy documents (e.g., from Australia and Ireland).
Even where good quality data exists, gender is often not recorded correctly, implicitly assuming all treatments are equal.
This is the same kind of issue that resulted in testosterone, a vital natural hormone, being plagued by safety concerns. A now infamous study claimed testosterone caused cardiovascular issues – but later revealed some of the patients were women. The TRAVERSE study has now corrected this, but at great cost. Better data from the beginning could have avoided this entirely.
2. What are the opportunities that we see?
We are very optimistic about the future of men’s health. Men are becoming more and more interested in preventative action around their health, and we can personally attest to the passion that exists in the medical community for this topic.
Each of the challenges mentioned above presents an opportunity to reduce the male life expectancy gap. We have suggested three below.
2A. Creation of a men’s health qualification for healthcare professionals to improve patient outcomes
Within a siloed system, each patient needs a champion – someone who is willing and able to take a step back as a “generalist” and identify the right next step on the diagnosis and treatment journey. We believe that GPs are well placed to fulfil this role in theory.
To address the identified stigma, myth and uncertainties regarding men’s health topics, we propose the creation of a standardised men’s health qualification for healthcare professionals. This structured qualification can be flexibly delivered online and follow well thought through structures that exist both in certain pockets of the UK and in other European countries.
Aside from being educational for healthcare professionals across many different specialities and tenures, it could also provide a point of differentiation as they attempt to build their relationships and reputation within their local community.
We believe this qualification would improve healthcare professionals’ awareness of and confidence in treating men’s health conditions, as well as referring on patients to other specialties appropriately.
2B. Broaden screening and treatment incentives for men’s health conditions
We propose an increase in the scope for current screening and treatment incentive plans as they relate to critical men’s health conditions. We suggest that screening, diagnosis and treatment of some key drivers of premature male mortality could be incentivised to great effect.
We propose that adapting existing healthcare screening protocols for men (including the Over 40s HealthCheck) to include PSA and testosterone blood tests would at worst provide a key baseline figure to return to in future years, and at best save lives. Screenings for younger demographics could also be targeted to address men in high-risk populations.
We further propose that adapting incentives around the treatment of erectile dysfunction, a well-documented early warning sign of cardiovascular disease, could have far reaching impact on both length and quality of life. Increasing the scope to increase diagnoses of other related conditions would also be relevant, e.g., low testosterone, prostate cancer.
2C. Set out clear metrics for success, tracked by a dedicated team
While other men’s health strategy documents have shied away from metrics, the UK can distinguish itself by laying out a clear, data-based mission, and associated alternative metrics. One approach would be to target the elimination of the men’s life expectancy gap by 2050, supported by a series of sub-objectives.
As shared earlier, the drivers of premature male mortality are not secret. Sub-objectives could relate tactically to key drivers – like obesity and smoking rates in boys and men. They could also relate to the number and impact of pilots conducted across the UK to help improve men’s health.
“You can’t manage what you can’t measure” – as such we propose that a dedicated research team would be crucial to measure impact. Well known measures like impact on QALYs (Quality Adjusted Life Years) could be put in place to assess which efforts are having the greatest effect.
The team could also conduct analysis on existing gendered datasets to help ideation and targeting of new pilots to positively contribute to men’s health. This is important as we know that some areas and communities have worse outcomes than others and should be prioritised accordingly. Without well-targeted efforts, we can continue to expect a postcode lottery impacting men’s life expectancy.
3. How can we help to deliver a successful Men’s Health Strategy?
Androlabs is well-positioned to support the delivery of a successful Men’s Health Strategy. As a pharmaceutical company dedicated to men’s health, our mission is to eliminate the male life expectancy gap. At face value, we propose to do this through further innovation of prescription medicines for men.
However, we have a range of other relevant opportunities to support, including through the below.
3A. Leverage our network of healthcare professionals across Europe to understand best in class practices
We have built trust-based relationships with healthcare professionals across Europe. We are very fortunate such that we can readily discuss with some of Europe’s top andrologists, urologists and endocrinologists.
We have already used these networks to conduct surveys of healthcare professionals to understand treatment decision making; and could readily do so again. These surveys could be formal or more informal “pulse-checks” of new proposals and ideas.
We have also developed from these relationships a deep appreciation for the different education and training regimes of healthcare professionals across countries – be it Harvard degree courses, endocrinology nurse training, andrology courses and more. We would be happy to compile our insights on the latest trends and the benefits and pitfalls of these different approaches for the benefit of the UK.
3B. Build awareness of andrology topics among healthcare professionals
We are fixated on raising awareness of andrology topics. Aside from dozens of meetings daily with healthcare professionals across Europe, we have taken opportunities to build new and engaging content and have much more to do.
For example, we established our Scientific Advisory Committee in 2022, a select group of specialists from across the continent. We have been able to share their insights with specialists across markets in a clear whitepaper (included as a separate attachment for information). We have also sponsored our first journal submission, coordinated by our SAC members, which is pending publication in the Andrology journal.
We are very proud to have provided down-to-earth summaries of key andrological topics across channels with high degrees of trust and formality (i.e., journal articles, white papers).
We are excited to expand our digital capabilities – to reach the thousands of healthcare professionals across Europe in more informal ways but with the same level of scientific rigour.
3C. Fight misinformation by supporting the free dissemination of quality men’s health content for patients
We have been exploring ways to increase awareness of key men’s health conditions while remaining non-promotional.
Our most recent initiative has been “The Brother’s Arms” – Britain’s first “Men’s Health Pub”. We asked ourselves, if men are not engaging with the health system, where can we bring health education to them? A survey of over 1000 men suggested the pub.
We brought together charities, healthcare professionals and brands to transform Westow House in Crystal Palace into Britain’s first men’s health pub. Over three weeks, we hosted seven events covering fatherhood, mental health, urology health and male hormones.
We conducted over 100 blood pressure checks and a specialist even diagnosed someone with low testosterone. More than 250 men and women attended. Three in four participants said they would change their health behaviour as a result.
By connecting health touchpoints to activities men are already engaging with, we can lower barriers to entry. This gets men to access healthcare when needed and hopefully prevents premature deaths. We are already exploring how we can grow the Brother’s Arms across the UK and into Europe and are happy to share more information about our plans.
We are also committed to the non-promotional online tool we built called “TRTed.org”. This website, available in multiple languages, is filled with non-promotional content and resources for patients – including the world’s first “Men’s Health Podcast”, available on Spotify.
Androlabs is excited to continue fighting misinformation and raising awareness of key men’s health conditions in novel and efficient ways.


